A man in his 30s living in Kannai visited Spine Chiropractic with neck pain accompanied by numbness in his arm.
(Note: The image is a free stock photo.)
He started having neck pain pretty often about two months ago, and over time it began to cause numbness in his left arm as well.
He first went to an orthopedic clinic near his home, where they took an X-ray and told him the space between C5 and C6 was narrowing (but he didn’t get an official diagnosis then). They gave him some pain medication.
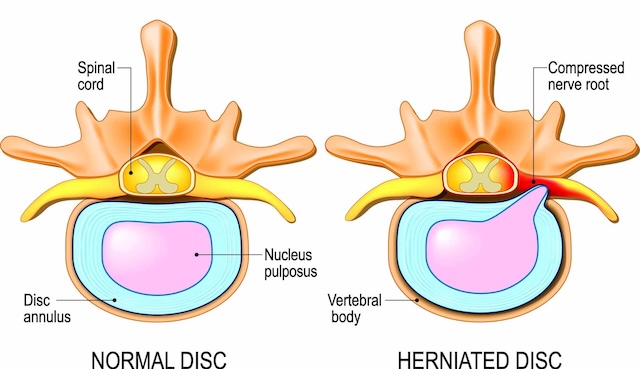
Since the pain didn’t get better, he went to a general hospital next. After getting an MRI, he was diagnosed with a cervical disc herniation. He was prescribed Voltaren, which he was still taking when he came to my clinic. The hospital suggested a nerve root block injection, but he felt uneasy about getting an injection in his neck. When he searched for other ways to improve his symptoms before going through with the injection, he came across Spine chiropractic and decided to give it a try.
[Initial Symptoms]
Interview:
His symptoms have been progressively worsening. About two weeks after he first began experiencing neck pain, numbness started to appear in his left arm. The numbness extends to the fingertips and is felt throughout the entire palm.
Neck movements aggravate the numbness, particularly when he tries to look upward, which significantly intensifies the sensation in his left hand.
He experiences the most severe neck pain upon waking in the morning. Although he has tried changing pillows and even sleeping without one, none of these adjustments have provided relief.
While taking the prescribed Voltaren does reduce the pain, it causes stomach discomfort, so he has been trying to limit its use as much as possible.
Visual Inspection:
During the consultation, the patient showed a rounded posture with forward-rolled shoulders, a posteriorly tilted pelvis, and a forward head position—typical characteristics of poor posture. (I suspected this was because tucking the chin worsened the symptoms.)
Static Palpation:
On palpation, there was noticeable tension in the muscles around both shoulders and the cervical region. Excessive tension was also observed in the muscles surrounding the left scapula, along with a tendency for the scapula to flare outward.
Motion Palpation:
He experienced radiating numbness into the arm with neck movements in any direction, but the symptoms were particularly provoked when he flexed his neck forward (looking downward).
Movements of the left arm itself did not significantly reproduce his symptoms.
Orthopedic Tests:
Cervical Compression Test (+):
Applying downward pressure on the cervical spine increased the numbness in the left arm.
Cervical Distraction Test (+):
Gentle traction of the cervical spine alleviated the numbness in the left arm.
Vertebral Artery Test (–):
This test, which screens for vertebral artery insufficiency affecting blood flow to the brain, was negative.
Myotome:
Left Shoulder Abduction (Deltoid): 3/5 – The patient is able to lift the arm independently, but cannot maintain the position when resistance is applied.
Dermatome:
Diminished sensation was noted along the left thumb side (C5–C6 dermatome).
Based on these neurological findings indicating reduced neural transmission in the C5–C6 cervical region, reflex testing was not performed. The treatment plan was established accordingly.
[Initial Treatment Plan]
The first treatment session was performed carefully while monitoring his response. Because the affected area showed low tolerance to stimulation and his symptoms fluctuated easily, direct treatment to the painful site was minimized. Instead, I focused on relaxing the muscular pathway associated with the arm numbness—from the cervical region through the shoulder and down toward the thumb.
For the cervical spine, I first assessed the range of motion to determine a safe treatment direction. Since cervical traction relieved the numbness in his arm, I based the treatment on decompression and performed traction therapy.
A follow-up visit was recommended three days later.
[Prognosis]
Second Visit (3 days later):
He visited after work, and we reviewed his condition over the past three days. After the previous treatment, his symptoms had improved to about 6/10, but they returned to the original level the following morning.
Since there was no post-treatment worsening, I proceeded with cervical treatment. In addition to traction therapy, I performed soft-tissue release on the sternocleidomastoid muscle, located at the front of the neck.
Third Visit (3 days later):
As with the previous visit, his symptoms eased slightly after treatment but had returned by the time he came in. However, his neck pain remained reduced. Because there were still no signs of worsening, I performed the same treatment protocol as before.
Fourth Visit (3 days later):
At this point, the effects of treatment were beginning to hold. By the time he visited three days later, his neck pain had eased, and the area of numbness in his left arm had begun to shrink.
Based on this progress, I extended the interval to one week.
Fifth Visit (1 week later):
Both the intensity and area of symptoms continued to gradually decrease. For the first time, I performed spinal adjustments—specifically to C2 in the upper cervical spine and to T3 in the prone position.
He experienced slight numbness after the adjustment, so I advised monitoring the symptoms.
Sixth Visit (1 week later):
The day after the previous treatment, the numbness briefly increased but then disappeared, and by the time he returned, he was feeling significantly better.
As cervical mobility had improved, I added cervical mobilization to address his straight-neck posture and help restore proper curvature.
Seventh Visit (1 week later):
His neck pain had settled considerably, and the numbness continued to improve. After performing the same treatment approach, I extended the interval to two weeks. He remains under ongoing observation.
[Practitioner’s Opinion]
Because a significant amount of time was required for examination during the first visit, the treatment session itself was kept brief. When a cervical disc herniation is suspected, symptoms can easily worsen with inappropriate care, making it essential to create a cautious treatment plan and carefully control treatment intensity.
Since this patient clearly presented with radicular symptoms, I avoided any cervical mobilization during the first session. Instead, I focused primarily on soft-tissue work aimed at relaxing the surrounding musculature, while placing greater emphasis on explaining the treatment plan and expected prognosis.
One of the most important considerations in treating disc herniation is preventing treatment-induced inflammatory reactions. Direct manipulation of the herniated segment is contraindicated and must be avoided.
From the perspective of Spine Chiropractic theory, herniation occurs when mechanical load—such as body weight (in this case, the weight of the head) or repetitive movement—continues to concentrate on a single point. Therefore, treatment aims to restore mobility and flexibility of the vertebrae above and below as well as the surrounding muscles, allowing load to be dispersed—much like a willow swaying in a storm.
In this case, the patient’s head position had shifted forward, and the reduced cervical curvature (straight-neck posture) caused the weight of the head to create vertical compression on the intervertebral discs.
Additionally, a left rotation at C5 was observed, which likely contributed to the disc herniation at that level.
Before performing any cervical adjustments, I observed his progress over five treatment sessions. Considering the risk of aggravation, I prioritized relaxing the surrounding tissues first and waited until an appropriate level of improvement and stability was confirmed.
Although the patient is still under observation, the fact that his condition allowed for treatment intervals to be safely extended to two weeks indicates that the chosen approach was appropriate. This case reinforces confidence in spinal chiropractic principles when managing suspected cervical disc herniation.
At Spine Chiropractic, I address a wide range of musculoskeletal conditions directly impacting daily life, not merely as a form of relaxation therapy. Conveniently located within a one-minute walk from Bashamichi Station, an eight-minute walk from Nihon-Odori Station, a seven-minute walk from JR Kannai Station, and a 12-minute walk from JR Sakuragicho Station, my clinic is well-suited for residents and workers in the Yokohama area.
If you are experiencing similar symptoms, please feel free to visit Spine Chiropractic. I am committed to providing care with sincerity and professionalism.