A man in his 40s, who works in the Kannai area, visited my clinic complaining of numbness in his right leg caused by a lumbar disc herniation.
The patient had a long history of chronic lower back pain, but the pain worsened about three months ago, accompanied by numbness radiating from the right buttock down the leg.
While sitting at work, the numbness in the buttock and leg gradually intensified, making it difficult for him to concentrate.
The pain was most severe in the morning, and getting out of bed each day was particularly difficult, so he began taking pain medication prescribed by his physician at night before going to sleep.
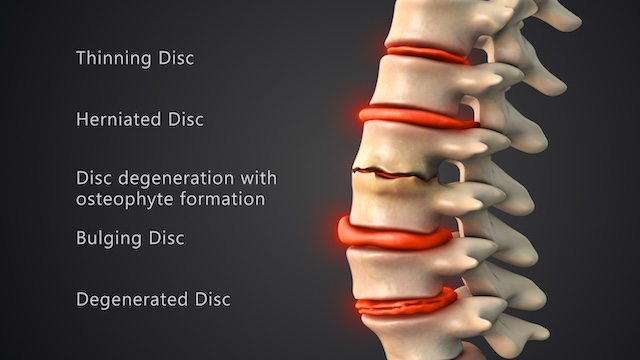
An MRI scan revealed lumbar disc herniations at the L4–L5 and L5–S1 levels.
He had been receiving medical treatment for the past three months, but as the pain did not improve with oral medication, he began to receive regular nerve root block injections.
These injections initially provided significant pain relief, giving him hope for improvement.
However, as the effect of the injections wore off, the pain gradually returned, and he found himself repeating the cycle of receiving further injections.
When he asked his physician whether there was a more fundamental solution, surgery was recommended.
Since he did not wish to undergo surgery, he decided to wait a little longer.
Looking for alternative treatment options, he searched online and discovered chiropractic care.
He then found my clinic located near his workplace and decided to visit Spine Chiropractic for treatment.
[Initial Symptoms]
Interview:
It had been a while since his last nerve root block injection, and during the consultation he was already reporting pain while sitting.
The pain was located in the right lower back and buttock, accompanied by a sensation of numbness in the back of the thigh.
Because of the pain, he tries to avoid bending forward as much as possible, and he has to be very careful each time he puts on underwear, pants, or shoes.
He is also cautious every time he stands up from a chair.
Visual Inspection:
During the consultation, he maintained a posture in which he slightly lifted his right side while sitting and standing.
Static Palpation:
Increased tension was observed in the right gluteal muscles and hamstrings, which was considered to be due to pain-induced muscle hypertonicity. A pronounced posterior displacement of the L4–L5 vertebrae and the sacrum (which would normally be positioned slightly anteriorly) was noted.
Motion Palpation:
Pain radiating from the buttock to the leg increased when the patient rotated the trunk to the right or bent to the right while seated. A similar response was noted in the standing position, though the leg numbness was less pronounced compared to when these movements were performed in a seated position.
The right hemipelvis appeared to be rotated posteriorly, and palpation of this area produced a slight reduction in the pain experienced in the lower back and buttock.
Orthopedic Tests:
- SLR (+): Straight-leg raise on the right side reproduced increased numbness in the leg when the leg was elevated in the supine position.
- DLR (+): Raising both legs simultaneously in the supine position elicited pain in the lumbar and gluteal regions, as well as increased numbness in the leg.
- WLR (–): The well-leg raise test, performed by lifting the unaffected leg and dorsiflexing the ankle, did not provoke pain.
- Kemp’s test (+): In the seated position, trunk rotation and lateral bending reproduced increased pain and numbness in the buttock and leg.
Muscle Strength Examination:
Since the above tests strongly indicated a lumbar disc issue, I didn’t carry out any further testing.
[Initial Treatment Plan]
The patient was able to lie prone in a flat position, so treatment was started from that posture.
With radicular symptoms, it is especially important to avoid aggravating the condition during treatment, so the treatment intensity must be adjusted gradually.
Specifically, I do not perform joint adjustments in the first session.
In many cases of radicular symptoms, inflammatory reactions are involved, and joint manipulation can potentially worsen the inflammation.
Therefore began by focusing on reducing irritation to the nerve root and its pathway (in this case, along the sciatic nerve).
I applied the Graston technique to release the fascia along the sciatic nerve pathway, followed by psoas muscle release in the supine position and release of the gluteus medius and minimus.
Only the above treatments were performed in the first session, and the patient returned for follow-up four days later.
[Prognosis]
Second Visit (4 days later):
The patient reported that symptoms had flared up the day after the first treatment but then subsided, with no significant improvement overall.
I suspected that releasing the gluteus minimus and psoas muscle in the first session had temporarily increased the load on the intervertebral disc.
However, I explained that restoring flexibility and enabling these muscles to support the body properly was ultimately beneficial, and I repeated the release work during this session.
To help control post-treatment inflammation, I concluded the session with ultrasound therapy.
Third Visit (3 days later):
The patient came in after work and was experiencing a flare-up of symptoms.
However, unlike after the first session, he reported no rebound pain the following day — likely due to the use of ultrasound therapy at the end of the previous session to suppress inflammation.
Since muscle tension around the lumbar region was still high, I again performed soft-tissue release and, this time, added spinal mobilization based on my clinic’s Joint Motion Theory, while avoiding direct stress on the affected disc area.
Fourth Visit (1 week later):
Since there had been slight improvement after the previous session, I extended the interval to one week.
However, the patient reported that the symptoms began to intensify again around the fourth day after the visit.
That said, the symptoms were comparatively milder than before, and the post-treatment flare-ups seen in earlier sessions were no longer present.
I therefore decided to continue with the same treatment approach once a week for the time being.
Fifth to Seventh Visits (1–2-week intervals):
During this period, adjustments were performed to the upper lumbar spine and the right sacroiliac joint (note: the diagnosed herniation was in the lower lumbar spine).
By improving spinal mobility, I aimed to redistribute mechanical load and reduce the stress concentrated on the herniated segment.
Eighth Visit (2 weeks later):
By this time, the frequency of symptom provocation had decreased significantly compared with the initial presentation.
The patient reported that symptoms were now limited to occasional flare-ups after prolonged sitting and that he was no longer taking any medication.
As of September 2025, I determined that the patient’s condition was stable enough to transition to a maintenance phase, and the active treatment phase was concluded.
[Practitioner’s Opinion]
This patient presented with symptoms that were typical of a suspected lumbar disc herniation.
The causes of disc herniation are multifactorial and may include:
- Weight gain
- Aging
- Lifestyle habits
- Occupational and environmental factors
- Reduced mobility of muscles and joints
- Nutritional factors
All of these play important roles, but in modern society, environmental factors such as prolonged sitting for desk work — along with the resulting lack of physical activity, decreased muscular support, and weight gain — place considerable stress on the intervertebral discs, particularly in the lumbar spine.
In this case as well, the patient’s condition was largely related to the cumulative stress from his work environment and insufficient physical activity, which had contributed to chronic low back pain over time.
He has now transitioned to a maintenance phase. Receiving treatment once every three to four weeks serves as support for maintaining his spinal health and preventing recurrence.
At Spine Chiropractic, I address a wide range of musculoskeletal conditions directly impacting daily life, not merely as a form of relaxation therapy. Conveniently located within a one-minute walk from Bashamichi Station, an eight-minute walk from Nihon-Odori Station, a seven-minute walk from JR Kannai Station, and a 12-minute walk from JR Sakuragicho Station, my clinic is well-suited for residents and workers in the Yokohama area.
If you are experiencing similar symptoms, please feel free to visit Spine Chiropractic. I am committed to providing care with sincerity and professionalism.