A male patient in his 40s visited my clinic complaining of pain extending from the right side of his jaw to his head.
A male patient began experiencing discomfort around his right temple approximately three months ago. While he had no difficulty opening or closing his mouth and was not in significant pain, he noticed a persistent sense of discomfort in his temporomandibular joint (TMJ).
Over time, the discomfort extended from his temple to the temporal region, developing into headache-like symptoms. Concerned, he visited a headache clinic, where an MRI scan was performed, confirming that there were no abnormalities. He was prescribed a nonsteroidal anti-inflammatory drug (NSAID) (aspirin) and a muscle relaxant (MioRelax) and continued this treatment with follow-up visits every two weeks.
Despite consistent medication, his symptoms did not improve. Additionally, as he began experiencing jaw pain, he consulted a dentist, who provided him with a custom-made mouthguard.
Initial Symptom Relief with a Mouthguard:
With regular use of the mouthguard, his morning headaches and jaw pain significantly improved. His dentist advised,
“Your symptoms are caused by jaw clenching, which is straining your jaw muscles and leading to headaches. Be sure to wear your mouthguard regularly.”
Following this advice, he continued to wear the mouthguard diligently.
Two months later, his morning symptoms remained resolved. However, as he could not wear the mouthguard during the day, he continued t experience headaches and jaw discomfort throughout the daytime.
Wanting to explore alternative treatment options beyond conservative therapy, he searched for other solutions. He discovered Spine Chiropractic in Bashamichi, which was conveniently located near his residence and listed ‘jaw pain’ as a treatable condition on its website. Hoping for a more effective approach, he decided to visit my clinic.
[Initial Symptoms]
- Interview: The patient reported that symptoms vary by day but occur an average of 2 to 3 times per week. While there is no pain while eating, pain tends to appear more frequently at night. It sometimes leads to headaches, and although the patient takes painkillers, they are ineffective. However, thanks to the mouthguard, morning headaches and jaw pain have improved. The pain is most commonly located from the right temple to the temporal region.
- Visual Inspection: No abnormalities were observed upon visual.
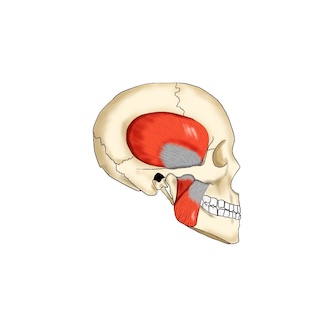
- Static Palpation: The right masseter muscle exhibits increased tension, and when compared to the left side, the right temporalis muscle appears slightly tighter with tenderness present.
- Motion Palpation: There is a slight discrepancy in the timing of the TMJ movement during mouth opening and closing.
- Opening: Right side lags behind.
- Closing: Right side moves faster.
- Orthopedic Tests: No specific diagnostic test is applicable.
- Muscle Strength Examination: Considering the relationship between symptoms, an examination of the sternocleidomastoid (SCM) muscle was performed. Even without measuring muscle strength, a noticeable asymmetry in tension was observed when lifting the neck. The right anterior neck exhibited significantly increased tension.
[Initial Treatment Plan]
The patient initially presented with headache as the primary complaint. However, based on history taking and palpation, it was determined that the headache was highly likely caused by bruxism-related muscle tension.
Treatment Approach:
The session focused on reducing tension in the muscles involved in clenching, including the masseter, temporalis, and mandibular muscle groups responsible for anterior-posterior jaw movement.
Additionally, the relationship between the frontal bone, occipital bone, and cervical spine was considered, as these structures contribute to muscle tension. While the TMJ moves primarily under the control of the mandible, it is functionally part of the maxilla-cranium complex and articulates with the first cervical vertebra (atlanto-occipital joint). Therefore, when treating TMJ issues, these structural components must be taken into account.
Poor posture, particularly cervical misalignment and straight neck (loss of cervical curve), is often a contributing factor. In this case, the patient’s symptoms were suspected to be related to forward head posture and straight neck syndrome.
For the first session, to carefully assess the patient’s response, high-intensity adjustments were avoided. Instead, the focus was placed on realigning the jaw-related musculature and cranial positioning, with minimal direct intervention on the temporalis muscle.
A postural correction plan was also included in the treatment strategy, which would be carried out over multiple sessions.
Since the patient is only available on weekends, they were advised to return in one week, and the session was concluded.
[Prognosis]
Second Session:
There was no significant change after the first treatment, but no worsening of symptoms either. Given this, the approach was adjusted to focus on:
Cranial adjustments
Restoring cervical lordosis (natural forward curve of the neck)
Fine-tuning TMJ opening and closing timing
Releasing tension in the temporalis muscle
The patient was advised to return in one week.
Third Session:
The patient was surprised to experience pain-free days for the first time in weeks. While headaches still occurred, their frequency had noticeably decreased. Seeing positive results, the same treatment approach was continued.
Fourth Session:
After another week, the headache symptoms had significantly reduced. While mild discomfort was still present at times, both the duration and frequency of pain had decreased. Based on this improvement, the treatment interval was extended to two weeks.
Fifth Session:
Upon returning after two weeks, the patient noted that headaches had increased slightly in the second week. In response, the treatment approach was expanded to include the upper back and lower back, focusing on postural correction to provide more stability.
Sixth Session:
With the addition of postural correction techniques, the patient was now able to maintain improvements over a two-week period. After two weeks, the pain level had decreased to less than half of what it was initially.
At this point, the chiropractic treatment phase was completed.
Maintenance Phase:
The patient transitioned to preventive care, receiving maintenance treatments every 3 to 4 weeks. Now, two years have passed since the initial visit, and the patient continues to receive regular care at Spine Chiropractic in Bashamichi.
[Practitioner’s Opinion]
This patient presented with coexisting symptoms of headaches and TMJ, conditions well-suited for chiropractic care. While nighttime bruxism (clenching and grinding) was improved through the use of a mouthguard, it did not address the underlying causes, leading to persistent daytime symptoms.
Root Causes & Treatment Approach
The headache and jaw pain were primarily due to excessive tension in the muscles involved in mastication (chewing). Therefore, treatment focused on:
Releasing tension in the overactive muscles
Addressing the underlying causes contributing to muscle tightness
In this case, the forward head posture led to increased tension in the posterior cervical muscles, contributing to discomfort. Additionally, work-related stress and environmental factors further exacerbated the symptoms.

Holistic Management
Though not previously mentioned, stress played a significant role in this case. Alongside chiropractic treatment, lifestyle modifications aimed at promoting mental relaxation were recommended, which the patient actively implemented.
Long-Term Outcome
The patient’s commitment to self-care was crucial in preventing recurrence. A notable factor was that he changed jobs, leading to a less stressful work environment, which significantly contributed to long-term symptom resolution.
This case highlights the importance of a comprehensive approach, where physical, postural, and psychological factors are addressed for lasting improvement.
At Spine Chiropractic, I address a wide range of musculoskeletal conditions directly impacting daily life, not merely as a form of relaxation therapy. Conveniently located within a one-minute walk from Bashamichi Station, an eight-minute walk from Nihon-Odori Station, a seven-minute walk from JR Kannai Station, and a 12-minute walk from JR Sakuragicho Station, my clinic is well-suited for residents and workers in the Yokohama area.
If you are experiencing similar symptoms, please feel free to visit Spine Chiropractic. I am committed to providing care with sincerity and professionalism.