A 50-year-old woman complained of Pain in the Sole of the Right Foot After Wearing Heels for More Than 30 Minutes
A female patient who frequently wears heels for work visited the clinic complaining of pain in the sole of her right foot.
Her company recently began encouraging in-office work four days a week, which led to her wearing work shoes, such as pumps or low heels, more often. Since then, she started experiencing pain in the sole of her right foot.
Interestingly, the pain is only present in the right foot. While the discomfort subsides when she is seated at her desk, it worsens during her commute or when moving around the office. By nighttime, she often experiences a dull ache, prompting her to use ice packs for relief.
As the pain persisted, she visited a local orthopedic clinic, where X-rays were taken. However, no abnormalities were found. The doctor diagnosed her with plantar fasciitis and prescribed painkillers, advising her to monitor the condition. She attended the clinic weekly but received no specific treatment. During her third visit, the doctor suggested trying insoles if the pain persisted. She purchased insoles but found them to increase her pain, so she stopped using them after a while.
After over a month of ongoing pain, she searched for solutions online and came across social media posts suggesting that acupuncture, osteopathy, or chiropractic care could be effective. Wanting to try one of these approaches, she decided to visit my clinic.
The patient expressed fear of needles, so she preferred not to try acupuncture. my clinic is her second attempt at seeking chiropractic or osteopathic treatment. She mentioned that if her condition doesn’t improve here, she plans to visit a larger hospital.
[Initial Symptoms]
Interview:
The pain is mostly concentrated on the medial (big toe) side of the right foot. At home, the pain gradually lessens when the affected foot is not in use, but walking consistently triggers discomfort. Athletic shoes, with their better cushioning, provide relief. On weekends and even on workdays, she changes into athletic shoes during her commute unless she has client meetings or similar obligations.
Visual Inspection:
Upon observation, it was immediately noticeable that when standing, her right knee rotates inward while the toes point outward. This observation hinted at the potential cause, which will be explained later.
Static Palpation:
Both in standing and supine positions, the right vastus medialis of the quadriceps showed high tension. (No significant difference in tension was noted during palpation in the seated position.)
In the standing position, both the medial portion of the right soleus and the right peroneus longus also exhibited increased tension.
Motion Palpation:
Knee Joint restricted external rotation movement in the right knee joint.
No other abnormalities observed.
Orthopedic Tests:
Tests performed from the hip joint to the ankle joint did not reveal any positive results under standard orthopedic testing methods.
However, the knee adduction test elicited tenderness at the pressure point on the medial side of the knee.
Muscle Strength Examination: Tibialis anterior muscle strength: Right 4/5. The patient demonstrated good strength but reported that generating force on the right side was more difficult compared to the left.
[Initial Treatment Plan]
The patient’s knee joint was observed to be positioned inward, and the toes were pointing outward. These misalignments were corrected during the session.
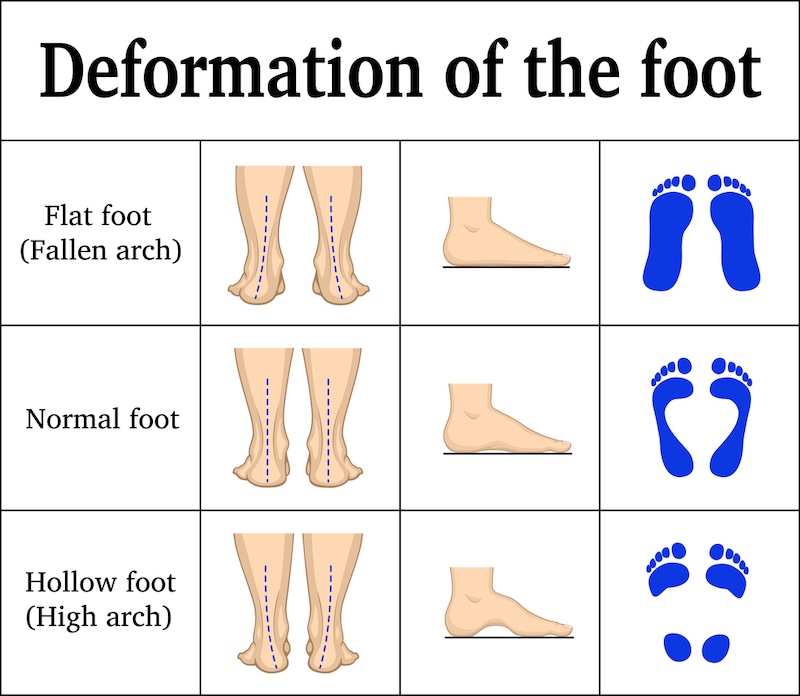
As shown in the diagram below, the condition resembled pronation; however, the issue was more complex. Specifically, the inward rotation of the knee combined with the outward rotation of the toes (this condition may be difficult to imagine from text alone) resulted in secondary effects. Fundamentally, it will be necessary to improve the positional relationships of the hip, knee, and ankle joints—including the pelvis—and incorporate training to help the patient properly recognize and maintain the correct alignment.
In the first session, we corrected the inward positioning of the knees and adjusted the joint misalignment of the feet, where the toes were pointing outward. Additionally, we performed techniques to relax the muscle groups that contribute to this joint positioning. This included the correction of joint alignment and releasing tension in the plantar fascia and the flexor muscles under it (responsible for toe flexion). The patient was instructed to return for a follow-up visit in five days.
[Prognosis]
[Second Session]
When asked about the condition following the first session, the patient reported that the pain returned on the way home, and there was little noticeable change. However, since it was still the initial treatment, it was too early to determine its effectiveness. Therefore, the same treatment was performed. The main difference from the first session was the addition of techniques targeting the hip joint and pelvis, aiming to address overall balance deviations. As with the previous session, the patient was instructed to return within a week.
[Third Session]
Upon her third visit, the patient reported that the pain had returned to the same level as before. However, unlike the first session, she experienced a few days of reduced pain after the second session. Similar to the previous session, treatment focused on addressing the symptoms from a comprehensive perspective. This time, taping was applied to the inner thigh muscles and the ankle joint after the session. Additionally, the patient was instructed on exercises targeting the outer foot muscles and the inner calf muscles. The next visit was scheduled for one week later.
[Fourth Session]
At the fourth session, the patient reported that the pain had been almost completely absent for the past week. While there was still a slight sense of discomfort, the pain had decreased to a 2–3/10 compared to the initial visit. The same treatment approach was applied, and the interval between sessions was extended to two weeks.
[Fifth Session]
Two weeks later, the patient reported that while pain returned during the second week, it was still about half as severe as it was during the initial visit.
The same treatment was continued, and improvement was observed in the positional relationship between the knee and ankle compared to the first session. The ability to maintain this improved alignment over two weeks appeared to contribute to the sustained improvement in symptoms.
The patient also seemed to be consistently performing the exercise therapy I had instructed her to do at home, which played a significant role in maintaining and improving their symptoms.
Additionally, I have been applying kinesiology taping at the end of each session. The patient has been practicing and implementing the taping techniques at home, which also seems to be helping sustain the effects of treatment.
Finally, as the changes in joint alignment have affected the patient’s gait, I recommended replacing their shoes to better support the new alignment.
Currently, the phase of “chiropractic treatment” aimed at improving symptoms every two weeks has concluded. The patient has transitioned to a maintenance phase, receiving my treatment every 3–4 weeks to monitor her condition.
[Practitioner’s Opinion]
During the initial consultation, I observed the patient’s posture in a standing position and noted that her toes were pointing outward while their knees were slightly rotated inward. Although the pain was localized in the plantar area, I determined that the root cause of the issue lay in the misalignment of the axes of the knee and ankle joints.
This was likely due to a habitual walking pattern, where the knees slightly turn inward, and the toes point outward while walking. As a result, excessive stress was placed on the inner side of the foot near the big toe, which triggered the current pain.
This case required a comprehensive approach, not only addressing the painful area itself but also considering the underlying question: “Why is this pain being triggered in the first place?” Treatment needed to be carried out with a holistic perspective.
At Spine Chiropractic, I address a wide range of musculoskeletal conditions directly impacting daily life, not merely as a form of relaxation therapy. Conveniently located within a one-minute walk from Bashamichi Station, an eight-minute walk from Nihon-Odori Station, a seven-minute walk from JR Kannai Station, and a 12-minute walk from JR Sakuragicho Station, my clinic is well-suited for residents and workers in the Yokohama area.
If you are experiencing similar symptoms, please feel free to visit Spine Chiropractic. I am committed to providing care with sincerity and professionalism.